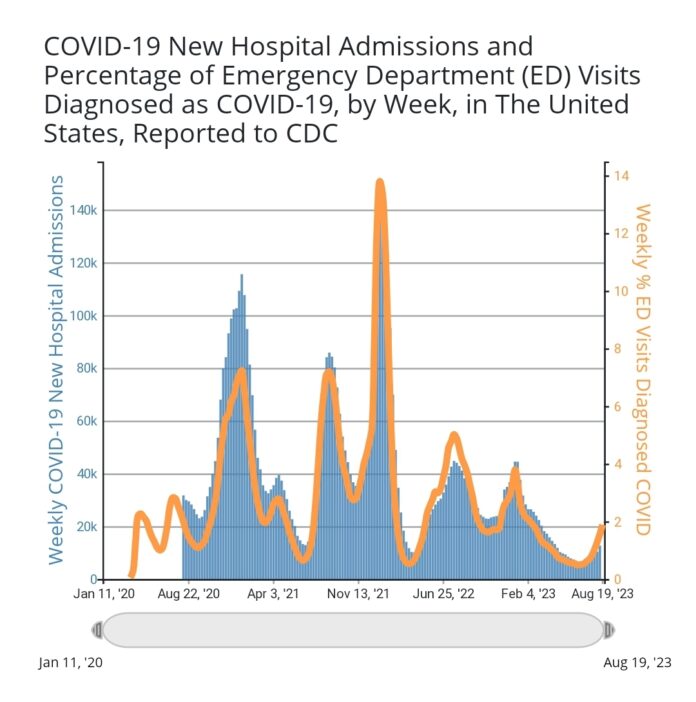
MURRAY – Media outlets have been documenting the slow proliferation of COVID-19 across the country for weeks. The Centers for Disease Control and Prevention (CDC) COVID Data Tracker shows a 21.6% increase in hospital admissions for the week ending Aug. 19 over the previous week; likewise, COVID-related deaths were up 21.4%.
Zooming in locally, even without any knowledge of the current metrics, much of the citizenry of Calloway County is aware, at least anecdotally, of the current surge in cases.
CDC’s county-level reporting shows 117 counties in the country where new hospital admission rates in their health service areas (HSA) are beginning to warrant attention, among them are the Purchase Area counties of Graves, Marshall, McCracken, Carlisle, Hickman and Ballard, which are all in the HSA serviced by Paducah hospitals Mercy Health-Lourdes and Baptist Health Paducah that, notably, does not include Calloway.
Murray-Calloway County Hospital’s Chief Nursing Officer Jeff Eye said that a surge in cases four to six weeks before the start of the school year has been typical for the past three years. This year is no exception.
Murray Medical Associates, who usually sees about 750 patients a week, saw closer to 900 patients last week, more than 350 of those were walk-ins; and they had 40 positive COVID patients. In addition, Murray Pediatrics reported around 20 cases. Eye also noted the clinics are receiving calls from patients who tested positive at home and are calling to report their results and receive guidance, adding those with mild symptoms can be managed at home.
But how is that impacting our local hospital? According to Eye, it isn’t. As of Tuesday morning, there was one patient hospitalized for COVID. “It will be like every other year; we’ll have to watch and see where we see impacts. We have had some staff out sick, and the clinics are very, very busy; but as of right now, the hospital is operating under normal conditions.”
The real question is: will it stay that way? Nationally, daily hospital admissions for COVID are expected to increase from 1,100 per day, as of Aug. 21, to 7,500 by Sept 18, according to an ensemble forecast – a combination of forecasts from independent teams – released by the CDC early last week.
The CDC characterizes the ensemble forecasting method as “among the most reliable forecasts in performance over time” but notes the forecasts “have not reliably predicted rapid changes in trends of reported cases, hospitalizations and deaths” and, therefore, should not be used as a decision-making tool.
For years, decision-making tools were based on case rates. Terms like incidence rate (the number of cases in a given period adjusted for population size), positivity rate (the percentage of positive results out of all tests administered) and seven-day rolling average (the average number of cases per day over a seven-day period) became part of the vernacular for many as they monitored conditions to make informed choices.
Over the course of the pandemic, the metrics used to monitor the impact of the virus on communities have changed. The CDC made clear when it released the Community Levels map in spring 2022 that its primary concern was to avoid stressing healthcare systems. That guidance was in stark contrast to the two years prior when minimizing community spread of the disease through monitoring case rates was the priority.
“When we were coming out of the emergency phase,” Eye explained, “the CDC said, ‘We’re not really worried about the prevalence of the disease in the community – we know it’s high – what we’re concerned about is the capacity of the hospitals to care for their communities, so we’re going to adjust our recommendations based on how well the hospital’s able to deal with the current disease burden and take care of the community. As long as the hospital’s fine, then we’re fine.’ Back up prior to that and they were doing positivity rate and prevalence rates to track how fast the disease was spreading in the community, anticipating that it would cause hospitalizations.”
Perhaps the most dramatic changes occurred after the federally-declared COVID Public Health Emergency (PHE) expired on May 11.
“The CDC and the Kentucky Department for Public Health (KDPH) data reports are going to change because much of the data that is needed to generate them will no longer be gathered or collected at the CDC,” Kentucky Public Health Commissioner Dr. Steven Stack explained during a press conference on May 11. “The COVID-19 community level map … will be removed from the website and be retired at the end of the business day today because we won’t be getting that data. The CDC won’t be able to generate that anymore.”
Since that time, CDC has, again, adjusted the primary surveillance indicators it uses to monitor COVID trends. Weekly COVID hospital admissions continue to be used along with the percentage of deaths from COVID out of all deaths in the United States. Hospitalization data remain the main metric for determining which mitigation strategies to employ, if any, on both personal and community levels, while mortality data provide insight on severity of illness.
“The CDC, regularly, will go back, look at old data and apply their new reporting model,” Eye said. “’If we had used this back then, would we have gotten the information that we needed?’ They’ll go back and rerun some of those reports, using the metrics they’re going to use moving forward, and say, ‘Does that line up with what we would have expected and how we would’ve issued guidance through that time period?’”
Through evaluating surveillance data sources and indicators from Oct. 1, 2020, to March 22, 2023, the CDC found that COVID hospital admission levels alone were still consistent with the Community Levels, which incorporated case rates. To that end, hospital admission rates only lagged one day behind case rates.
Mortality data are now sourced from the National Vital Statistics System. The CDC found those data strongly correlated with the aggregate death data previously used for tracking purposes and were 13 days timelier.
“They’re going to use provisional death certificates from the state, instead of a hospital saying, ‘We had a death of a patient who had COVID today’ because that’s what was happening,” Eye explained. “Some states would just report that number – this many people died, and on the day of their death, they had a positive COVID diagnosis. Our state, Kentucky, would go back and scrub those and say, ‘Did COVID appear to be contributable to their death?’”
“I’m proud of this,” Stack said of KDPH’s scrutiny of deaths deemed COVID-related. “It was very difficult along the way, but we have been very, very diligent in making sure that we reviewed all the cases that were outliers, that weren’t clear, to make sure we had folks who felt confident that we were including only people who died from COVID and not others. That process will now be mainstreamed into the normal process that we do for all death/mortality reporting. So, it won’t be quite the same in that we won’t have weekly data being reported, but (it will be reported) at least monthly and it will become more normal.”
But we learned over the course of the pandemic that hospitalizations and deaths are not leading indicators; in other words, hospitalizations and deaths only increase after a surge in cases is already underway. So, how do we know when cases are starting to climb now?
The CDC uses data collected through emergency rooms to detect early trends, specifically, the percentages of positive SARS-CoV-2 lab tests and emergency department visits related to COVID. In its evaluation of surveillance data, the CDC also found these ER metrics can identify trends four days earlier than hospital admissions.
“If you’re not going to do widespread testing, then the three places you would watch would be doctor’s offices, urgent care (clinics) and emergency departments,” Eye said. “That’s where you would look for the early indicators that you’re seeing an increase in COVID activity in a community. It would show up in one of those three places because that’s where people go, right? You’ll catch people with a little sniffle; you’ll catch people who are more short of breath; you’re going to catch people that have more severe illness and get admitted.
“You need all of those to paint a full picture, but if you’re trying to limit the amount that you’re having to track and report, and you’re out of that acute emergency phase, the approach makes sense. That is similar to what they have done historically for the flu. Emergency departments report the number of influenza-like illnesses and their total volume of ER visits.”
In addition to monitoring those four primary indicators, CDC will continue to use national genomic surveillance and wastewater surveillance to identify and monitor emerging variants.
Given the evolution of surveillance methods throughout the course of the pandemic, one pertinent question remains: are we better off now than we were three and a half years ago?
“Pre-COVID, we did not have a very robust surveillance system for monitoring infectious diseases across the country,” Eye explained. “When COVID started, at one point, we were reporting to four different agencies on four different platforms, and they all wanted different things. There was just a laundry list of things we had to report, 62 data elements every day.
“In December 2022, everything went back to NHSN (National Healthcare Safety Network), which is the data platform that we reported things on prior to COVID. There’s a list of things – MRSA, c-diff, central line infections, post-op surgical site infections, any reportable disease – that, any time we diagnose somebody with, we have to report it to the health department and the CDC. But it was still every day, as opposed to everything else, which is reported monthly.
“I wonder, in retrospect, if they think, ‘Why didn’t we just expand the NHSN reporting as opposed to three different government agencies developing three different platforms to report all of this stuff?’ And part of it was just that the system wasn’t well-coordinated.”
Since the PHE ended, the reporting burden on hospitals has dropped to 44 metrics that are reported weekly. Eye noted that, still, several of the data elements reported are not COVID-specific, such as supply levels and available beds.
“They may keep that up until they find a better way to keep tabs on hospital capacity,” he added. “They may be viewing that as ‘we needed to be doing that anyway, so we’ll just keep it.’ Because prior to COVID, they didn’t track any of that.”
In May, Stack told reporters that, while the country’s disease surveillance systems have improved over the course of the pandemic, there is still more that needs to be done.
“We need to build a strong nationwide system where information flows freely so that we can provide real time updates to the public on our websites so that you can be informed and you have confidence in that,” he said. “There’s a lot of work underway, but it’s complicated – there’s 50 states, nine territories, the District of Columbia and national government – and things are all politicized, as we’ve all seen. So, it’s difficult, but yeah, we’ve made progress.
“Wastewater testing holds promise to be able to find diseases earlier than we otherwise would have. Opportunities to maintain some form of hospital data reporting so that we have a sense of health care capacity, that’s important. I think we learned that that was valuable. … I think we’ve learned a lot, and I think we’ll make some meaningful progress on that (in the future).”
He also noted his hope to replace the state’s COVID website (kycovid19.ky.gov) with one focused more broadly on fall and winter respiratory illnesses, such as RSV and influenza, in addition to COVID. For now, KDPH still provides COVID-related data through two interactive dashboards – one for cases and deaths and one for vaccinations.
“For most of us, life already returned to our new normal a long time ago,” Stack said as he closed his prepared remarks. “For those of us later in life or with substantial medical conditions, ready access to high quality masks, tests, immunizations, treatments and adequate hospital care ensures that you can reduce your risk and more safely get treated and cared for, if you have COVID-19, to avoid bad complications.
“Even so, we would be wise to be mindful that COVID-19 has not gone and will not disappear. Remaining vigilant and supportive of each other is really important. And though it will be done less prominently, the Kentucky Department for Public Health will continue to monitor trends, keep the governor informed and make sure we share with you important updates as they occur.”